Abstract
Introduction
T-repleted haplotype mismatched (haplo) hematopoietic stem cell transplant (haplo-HSCT) from a relative has emerged during the last decade as a new modality of allogeneic transplant (allo-HSCT). The use of post-transplant high-dose cyclophosphamide (PT-HDCY) has been successfully introduced by the Johns Hopkins team. Initially this modality encompassed with non-myeloablative conditioning (NMAC) and bone marrow (BM) as stem cell source followed by post-transplantation GCSF (PT-GCSF) until engraftment. Then some teams investigated alternatives with more intensive preparation, either reduced intensity (RIC) or myeloablative (MAC) conditionings as well as the use of peripheral blood stem cells (haplo-PBSCT). In the latter situation, GCSF was usually kept contrary to what is usually done after HLA-matched PBSCT. In a cohort of 58 successive patients treated with haplo-PBSCT followed with PT-HDCY we did not administer any in-vivo GCSF. In this retrospective study, we compared the results of this cohort with an historical control group of 173 haplo-PBSCT treated with PT-GCSF.
Materials and methods
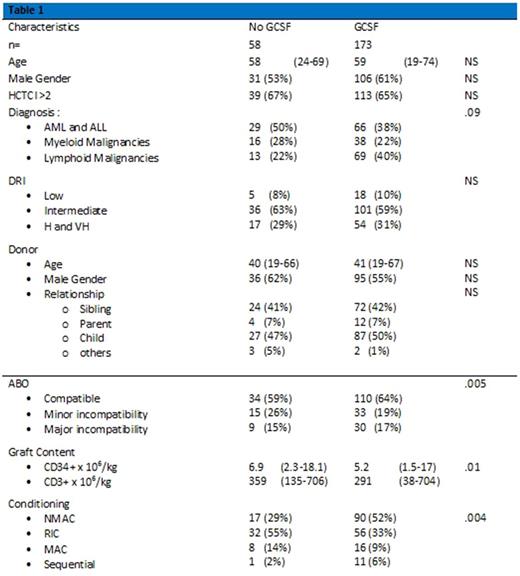
The goal of the study was to assess the impact of PT-GCSF on neutrophil and platelet recovery, and to evaluate the impact on overall survival (OS), progression-free survival (PFS), non-relapse mortality (NRM), incidence of relapse (IR) and incidence of acute/chronic GVHD. Patients' characteristics of both cohorts are resumed in Table 1.
Median time to neutrophils recovery (ANC >500 x106/L) was d+ 25 (range 15-43) in the group not treated with PT-GCSF, versus d+21 (range 13-112) in the control group (p .006) while platelet recovery (PLT > 20 G x 109/L) was achieved at d+29.5 (range 13-169) and d+32 (range 10-394), respectively (p 0.03). One-year OS and PFS in the study group were 63% and 65% respectively, versus 71% and 64% in the historical cohort (OS: p 0.2; PFS: p 0.8). The analysis of 1-year NRM (27% vs18%, p 0.3) or incidence of relapse (7% vs17%, p 0.3) showed no significant difference.
One-year cumulative incidence of grade II-IV aGVHD was 26% in the study group versus 20% in the control cohort (p 0.2) while the incidence of moderate-severe cGVHD was 10% versus 19%, respectively (p 0.05).
Conclusions
We conclude that PT-GCSF post haploidentical PBSCT significantly enhances the time for neutrophils recovery.
These results, however, doesn't seem having any significant impact on OS, PFS, NRM, IR or acute GVHD incidence.
Despite de small number of patients and the limitations of a retrospective study, we found a trend in cGVHD incidence, with patients who never received GCSF support experiencing a slightly higher rate of moderate-severe cGVHD.
These results, however, need to be further confirmed in larger studies or, possibly, randomized clinical trials.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal